Understanding Medication Administration Records
Medication Administration Records (MARs) are crucial documents in healthcare settings, serving as the backbone of medication management. A Medication administration record is not merely a compliance tool; it acts as a standardized record that organizes essential information about a patient’s prescribed medications. By utilizing a structured format, healthcare professionals ensure that every detail regarding medication use is documented clearly, reducing the likelihood of errors and enhancing patient safety.
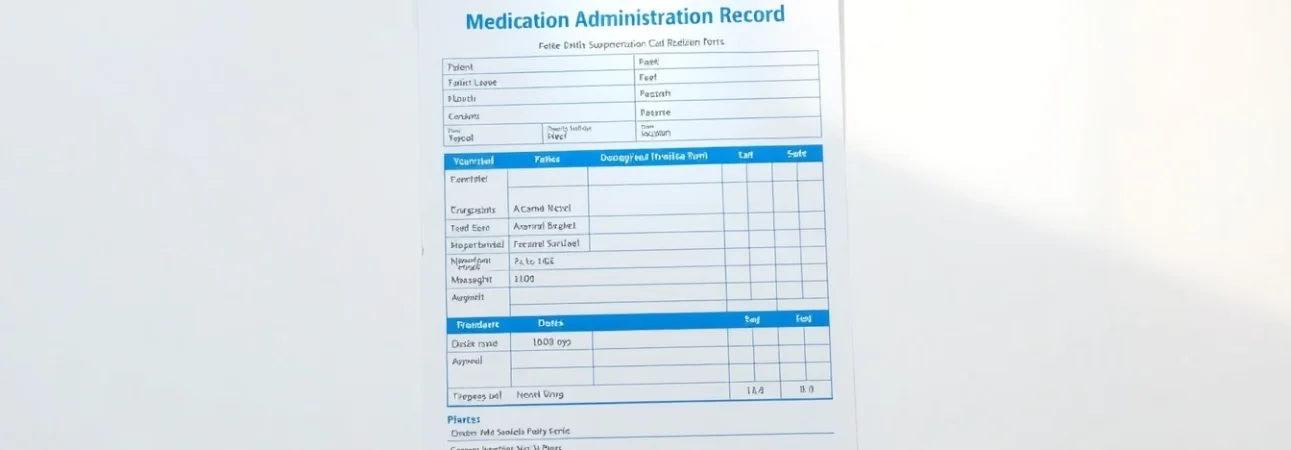
What is a Medication Administration Record?
A Medication Administration Record (MAR) is a legal document that provides a thorough protocol for administering medication to patients. This record typically includes details such as the medication name, dosage, route of administration, special instructions, and the time and date of each dose. The MAR serves not only as a log but also as a guide to ensure correct dosage and adherence to prescribed treatment plans. By capturing each of these critical data points, healthcare providers can monitor patient adherence to therapy and respond quickly to any adverse reactions or medication errors.
Importance of Accurate MAR Documentation
The accuracy of MAR documentation is vital for several reasons. It plays an essential role in:
- Patient Safety: Accurate records decrease the chances of medication errors such as overdoses, missed doses, or drug interactions.
- Legal Accountability: In case of disputes regarding medication errors, a well-maintained MAR can serve as legal evidence of compliance with medication administration protocols.
- Care Coordination: MARs facilitate communication between healthcare providers, ensuring that all parties are aware of a patient’s medications and administration schedules.
- Quality Control: Regular audits of MAR documentation can help identify trends related to medication administration and adherence, providing a basis for process improvements.
Common Components of an Effective MAR
An effective Medication Administration Record should include several key components:
- Patient Information: This includes full name, date of birth, and identifying number to ensure accurate tracking.
- Medication Details: Each entry should detail the medication name, strength, route of administration, frequency, and special instructions.
- Date and Time: Records should indicate when medication is administered and the timeframe for the next dose.
- Administering Personnel: Initials or signatures of the healthcare worker administering the medication should be documented.
- Observations: Any observations or adverse reactions following administration should also be noted for ongoing patient safety.
Best Practices for Utilizing Medication Administration Records
How to Properly Fill Out a Medication Administration Record
Filling out a Medication Administration Record correctly is imperative for ensuring patient safety and compliance with healthcare regulations. Here are some best practices:
- Use Clear Handwriting: If the MAR is a paper document, it’s essential to use legible handwriting to avoid misinterpretation of critical information.
- Follow Standard Abbreviations: Familiarize yourself with accepted medical abbreviations to maintain consistency throughout the records.
- Double-check Entries: Before submitting an MAR, review it for any discrepancies or incomplete information.
- Sign and Date Timely: Ensure to sign and date each entry at the time of administration to maintain an accurate timeline.
- Report Errors Immediately: If an error is identified after completing an MAR, it is crucial to report it to the overseeing physician or nursing personnel right away.
Ensuring Compliance with MAR Guidelines
Compliance with MAR guidelines is critical for maintaining the legal integrity of healthcare practices. Compliance can be enhanced through:
- Regular Training: Ensuring all staff are trained on MAR protocols is essential in promoting proper documentation and administration practices.
- Conducting Audits: Performing periodic audits on MAR documentation can reveal compliance trends and areas for improvement.
- Utilizing Checklists: Implementing checklists for medication administration can further ensure that all necessary steps are followed and documented efficiently.
- Feedback Mechanisms: Establish a process where staff can provide feedback on MAR usage and suggest improvements to practices.
How to Minimize Errors in MAR Documentation
Minimizing errors in MAR documentation calls for a proactive approach. The following strategies can be employed:
- Standardize Templates: Use standardized MAR templates that include all necessary fields and instructions, reducing variability and confusion.
- Implement Technology Solutions: Incorporate technology such as electronic health record systems to automate documentation and reduce human error.
- Encourage Reporting: Cultivate an open environment where staff feel safe reporting near-misses or errors without fear of reprimand.
- Practice Double-Checks: Encourage a culture where two individuals verify MAR entries and medication before administration.
Technological Innovations in MAR Management
Digital vs. Traditional Medication Administration Records
The evolution of technology has drastically changed the landscape of MAR management. Traditional paper MARs can often lead to misplacement and illegibility, while digital MAR systems offer numerous advantages:
- Accessibility: Digital systems allow for easier access from multiple locations and by various healthcare personnel, ensuring continuity of care.
- Real-Time Updates: Changes to a patient’s medication regimen can be made in real-time, reducing delays and risks associated with outdated entries.
- Integrated Alerts: Digital MARs can feature built-in alerts for potential drug interactions and other critical notifications, enhancing patient safety.
Benefits of Electronic Medication Administration Records
There are several benefits associated with electronic MARs, which include:
- Increased Efficiency: Electronic systems reduce the time healthcare providers spend filling out records, allowing more time for patient care.
- Improved Accuracy: Automated systems reduce the opportunities for human error and ensure that records are consistently filled out according to established guidelines.
- Data Collection: Electronic records facilitate more robust data collection, allowing health organizations to analyze medication usage trends and patient outcomes over time.
Integrating MAR Systems with EHRs
Integrating MAR systems with Electronic Health Records (EHRs) enhances the efficiency and safety of medication administration. This integration allows for:
- Comprehensive Patient Profiles: Healthcare providers can view all aspects of a patient’s medical history, prescriptions, and laboratory results in one location.
- Seamless Communication: Providers can communicate changes in medication directly through the EHR to all stakeholders involved in a patient’s care.
- Better Compliance Tracking: Organizations can more easily track compliance with medication regimens and identify areas of concern, ensuring patients receive the best care possible.
Challenges Associated with Medication Administration Records
Common Pitfalls in MAR Management
Despite the benefits of MARs, several challenges can impede effective medication administration:
- Inconsistent Training: Variations in staff training can lead to discrepancies in how MARs are completed, increasing the risk of errors.
- Underreporting Errors: There may be a reluctance among staff to report errors or near-misses, leading to a culture of silence and recurring issues.
- Time Constraints: High workloads may pressure healthcare workers to rush through documentation, which can lead to increased mistakes.
Addressing Non-compliance Risks with MARs
Addressing risks related to non-compliance with MAR documentation requires an organization’s commitment to quality improvement and regular monitoring:
- Developing Clear Policies: Establishing clear protocols for MAR usage and documentation can help set expectations for staff.
- Providing Continuous Education: Ongoing education and training programs can help reinforce best practices and the importance of following protocols.
- Conducting Regular Audits: Frequent reviews and audits of MAR records can identify noncompliance patterns and target areas for improvement.
Case Studies on MAR Fails and Lessons Learned
Case studies provide valuable insights into the repercussions of poor MAR management. One notable example involves a healthcare facility where an incomplete MAR led to a patient receiving a potentially harmful medication dose. The consequences were severe, resulting in prolonged hospitalization. This case highlighted the need for stringent MAR oversight and compliance standards, leading to subsequent training initiatives and the implementation of an electronic MAR system.
Learning from such incidents emphasizes the necessity of maintaining thorough, accurate records and dedicating resources to ongoing education and technology upgrades.
The Future of Medication Administration Records
Emerging Trends in MAR Management
The future of MAR management is leaning towards increased digitalization and integration with other clinical systems. Key trends include:
- Artificial Intelligence: AI-powered systems that can predict potential medication interactions are becoming increasingly common, offering a higher level of protection for patients.
- Telehealth Integration: As telehealth becomes more prevalent, the integration of MAR systems to facilitate remote patient monitoring and medication adjustment will become essential.
- Patient Engagement Tools: Systems that allow patients to access their MARs can encourage involvement in their own medication management and adherence to prescribed regimens.
Preparing for the Future of Electronic MARs
As the healthcare landscape changes, preparing for future electronic MAR systems involves:
- Investing in Infrastructure: Institutions need to prioritize robust digital infrastructure to support advanced MAR systems.
- Adapting to Regulatory Changes: Staying informed about changes in healthcare regulations regarding MARs will ensure compliance and continued funding for improvements.
- Fostering a Culture of Safety: Establishing an organizational culture focused on patient safety and quality care will be crucial in adopting new technologies effectively.
Continuing Education on MAR Best Practices
Ongoing education is essential to maintain the highest standards of MAR management. Best practices include:
- Regular Workshops: Arranging periodic workshops can serve as a platform for refreshers on MAR documentation.
- Utilizing e-Learning Resources: Leveraging online platforms for MAR training can make education more accessible and varied.
- Sharing Best Practices: Encourage healthcare personnel to share insights and strategies related to MAR documentation to foster community learning.